Creator attribution: Nick Youngson – link to – http://nyphotographic.com/ Source: http://www.thebluediamondgallery.com/a/assisted-dying.html
Paul Teed, University of Bristol
Assisted dying can be a divisive and polarising subject. But there is one aspect on which most people probably agree – the need to improve the conversations people have about death.
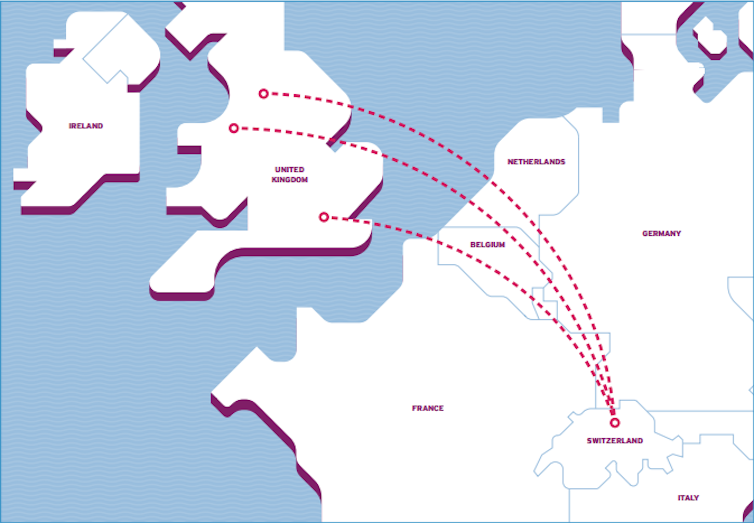
At the moment, there is uncertainty in the UK regarding what people – especially health professionals – can and cannot say when the topic of assisted dying comes up. Conversation can become especially stilted when it turns to patients obtaining the medical documentation required for an assisted death abroad.The situation requires clarification. Currently, if a doctor in the UK writes a specific report to help with an assisted death abroad (three organisations in Switzerland accept UK citizens), the General Medical Council (GMC) may view this as a “fitness to practice” issue.
However, if a doctor provides copies of medical records, even with the knowledge that they will be used for an assisted death, it is not a fitness to practice issue. The GMC’s position is that this would be “too far removed from the act of suicide to constitute encouragement or assistance”. Yet the doctor can still refuse this request for documentation. (The patient can then appeal to the information commissioner under the Data Protection Act 1998, but this may be unsuccessful.)
The desire to hasten death affects a significant proportion of dying people – not just the small proportion who undergo an assisted death. In places where a form of assistance to die is legal, such as the US state of Oregon, just 10-20% have their request agreed to. The ability to talk about these desires and the presence of an option can “make the future feel navigable”.
It is hard to measure how common a desire to hasten death is. One study revealed it was up to 11% within people in a UK hospice. The meaning behind this desire is varied, ranging from an avenue to begin talking about dying more generally through to wanting greater control.
I started my own research after noticing two major barriers in the conversations about assisted dying between doctors and patients. First, the Swiss organisations advise applicants not to divulge the reason for a request for medical documents due to the risk of refusal. Second, the uncertainty surrounding professional guidance means patients are not telling doctors about their plans or fears (and they may not be asked about them).
These barriers are affecting the crucial therapeutic alliance between doctor and patient. They also remove opportunities to highlight the specific needs of the dying. The fact that people change their mind about hastening their death is a reason to address their fears upfront – not push them away or ignore them. Yes, end-of-life care needs more funding, but this is of no use if those that need it do not feel they can be heard.
Sadly, this is what is borne out in Dignity in Dying’s recent publication The True Cost: How the UK Outsources Death to Dignitas. The report revealed a large discrepancy between those who felt they should be able to discuss these desires (82%) with those who felt that they would (32%). One respondent commented:
I wish there was somebody that was medical that you could talk to and [who could] explain … I just wish there were people you could talk to.
Another recalled a doctor saying: “You know you can’t talk about this sort of thing.”
Dying to talk
Throughout the publication runs a desire for openness to be able to talk about thoughts they are having, researching and acting upon. Instead, people encounter systemic obstruction, disapproving prejudgement and arbitrary practices. At its worst, the document highlights active silencing of these voices – people being told they mustn’t talk about assisted dying with anyone involved in their care.
Being able to talk openly about a desire to hasten death serves a vital palliative and therapeutic function. The opportunity to discuss perceptions of dying on the patient’s – rather than the profession’s – terms would help people to consider what it means (for them) to die. It could also serve to reaffirm social bonds, empower self-identity and give a voice to suffering.
Yet currently, people are possibly going abroad to die without ever talking to a healthcare professional about it.
Everyone wants to work towards getting our only experience of death right. For this to occur, the medical profession must avoid its dominance over end-of-life discussions, and seek instead to address the concerns of the dying – whatever they are. If not, the harm caused by the current fudge of legislative and professional guidance will not only go unrecognised, it will grow.
Listening and discussing requests to hasten death is not remotely illegal. The GMC itself states that doctors should “be prepared to listen and to discuss the reasons for the patient’s request”.
Improving these conversations is an urgent middle ground that both sides of the assisted dying debate can surely agree on. It is vital that the voices of the dying are heard.
Paul Teed, PhD candidate, School of Population Health Sciences, Bristol Medical School, University of Bristol
![]() This article was originally published on The Conversation. Read the original article.
This article was originally published on The Conversation. Read the original article.